October 6, 2014
Angiosomes in Critical Limb Ischemia
Critical limb ischemia is ischemic rest pain and / or nonhealing wounds of the lower extremity due to reduced arterial perfusion (1). Patients with critical limb ischemia are at elevated risk for amputation (2). Revascularization is an accepted treatment for patients with critical limb ischemia, when the goal is limb salvage, to improve perfusion and wound healing. Traditionally, restoring in-line flow to the foot via any tibioperoneal artery was thought to be sufficient for wound healing. However, more recently, there has been interest in pursuing revascularization of particular tibioperoneal and pedal arteries, depending on the vessel’s relationship to the wound (Figure – Click to enlarge). That is, target vessel revascularization is based on the ‘angiosome concept’.
1A, B) Left below-knee angiogram showing critically diseased anterior tibial artery supplying a dorsalis pedis artery, patent peroneal artery, and distally occluded posterior tibial artery. 1C, D) Since the nonhealing wound was felt to be in the angiosome of the posterior tibial artery, this vessel was revascularized.
The figure is from a case of an 85 year-old man with nonhealing, left heel wound for 6 months. The wound was located on the medial plantar surface of the heel. After the procedure wound healing was achieved.
What is the Angiosome Concept
The lower leg and foot can be divided into 6 regions or angiosomes based on arterial blood supply (table) (3).
| Region of limb | Arterial blood supply |
| Posterior calf | Posterior tibial |
| Anterior leg and dorsal foot | Anterior tibial and dorsalis pedis |
| Lateral ankle | Peroneal |
| Lateral heel | Calcaneal branches of peroneal |
| Medial heel | Calcaneal branches of posterior tibial |
| Plantar surface of the foot | Lateral and medial plantars (branches of posterior tibial) |
Following the angiosome concept, if a patient has a wound on the dorsum of the 1st toe, the anterior tibial and dorsalis pedis arteries would be the preferred vessels to revascularize.
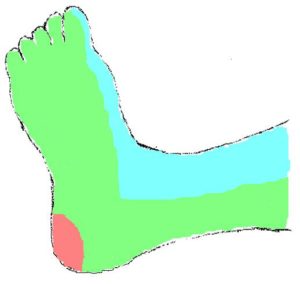
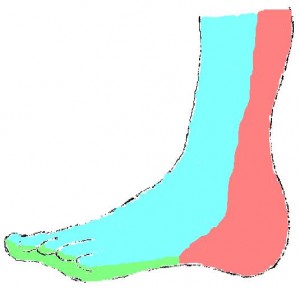
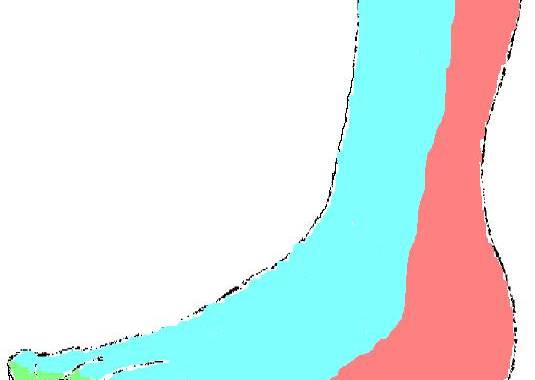
The following cartoons show the foot and ankle angiosomes (click to enlarge):
Evidence Regarding the Angiosome Concept
There are no randomized data for angiosome-guided revascularization and little observational evidence. In a retrospective study of 329 patients with critical limb ischemia followed for a mean of 18 months, those who underwent revascularization according the angiosome concept had more favorable limb outcomes (4). After propensity score matching, freedom from amputation was 82% +/-5% for limbs that were successfully revascularized according to the angiosome concept but 68% +/-5% (p=0.01) for the group with indirect revascularization (4). Similar benefits were seen in a retrospective series of 48 patients with non-healing wounds who underwent tibioperoneal bypass (5).
Limitations of the angiosome concept
First, more evidence is needed to firmly support angiosome-guided revascularization. Second, it is not always technically feasible to revascularize the artery supplying a wound. Third, the ability to achieve revascularization in the angiosome of interest may be a surrogate for less severe disease, rather than a sign of true therapeutic benefit. Despite these limitations, it is our practice to pursue angiosome-guided revascularization if technically feasible based on the available evidence and the biologic plausibility of clinical benefit.
References about angiosomes
- Slovut DP, Sullivan TM. Critical limb ischemia: medical and surgical management. Vascular medicine. 2008;13(3):281-91.
- Belch J, Hiatt WR, Baumgartner I, Driver IV, Nikol S, Norgren L, et al. Effect of fibroblast growth factor NV1FGF on amputation and death: a randomised placebo-controlled trial of gene therapy in critical limb ischaemia. Lancet. 2011;377(9781):1929-37.
- Yan BP, Moran D, Hynes BG, Kiernan TJ, Yu CM. Advances in endovascular treatment of critical limb ischemia. Circulation journal : official journal of the Japanese Circulation Society. 2011;75(4):756-65.
- Iida O, Soga Y, Hirano K, Kawasaki D, Suzuki K, Miyashita Y, et al. Long-term results of direct and indirect endovascular revascularization based on the angiosome concept in patients with critical limb ischemia presenting with isolated below-the-knee lesions. Journal of vascular surgery. 2012;55(2):363-70 e5.
- Neville RF, Attinger CE, Bulan EJ, Ducic I, Thomassen M, Sidawy AN. Revascularization of a specific angiosome for limb salvage: does the target artery matter? Annals of vascular surgery. 2009;23(3):367-73.