November 7, 2020
Intravascular Lithotripsy for Peripheral Artery Calcification: 30-Day Outcomes from the Randomized Disrupt PAD III Trial
Presented by William A. Gray, MD
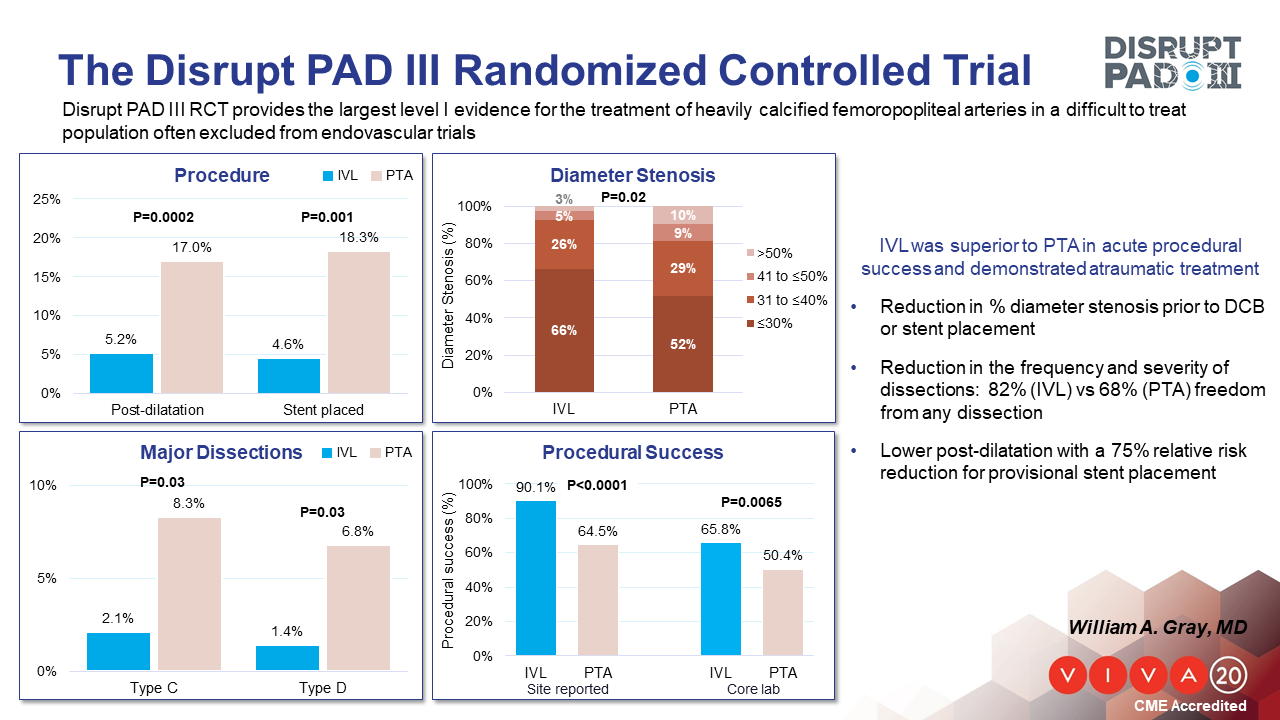
Endovascular treatment of calcified peripheral artery lesions may be associated with suboptimal vessel expansion, increased complication risk, and reduced long-term patency. Single-arm studies have reported promising results with intravascular lithotripsy (IVL) in the presence of moderate and severe calcium, yet comparative evidence from randomized trials is lacking.
The purpose of this study is to compare acute outcomes in patients receiving vessel preparation with IVL or percutaneous transluminal angioplasty (PTA) prior to drug-coated balloon (DCB) treatment for peripheral artery disease (PAD) in calcified femoropopliteal arteries. The Disrupt PAD III randomized trial enrolled PAD patients with moderate and severe calcification in a femoropopliteal artery who underwent vessel preparation with IVL or PTA. The primary effectiveness endpoint was procedural success, defined as core-lab adjudicated residual stenosis ≤30% without flow-limiting dissection prior to DCB or stenting. Secondary endpoints evaluated at 30 days included major adverse events (MAE) and clinically-driven target lesion revascularization (CD-TLR).
In patients receiving IVL (n=153) or PTA (n=153), the primary effectiveness endpoint of procedural success was significantly greater in the IVL group (65.8% vs. 50.4%, p=0.007). Post-treatment balloon dilatation (measured prior to DCB) residual diameter stenosis (27.3 ± 11.5% vs. 30.5 ± 13.9%, p=0.04), freedom from any dissection (81.5% vs. 67.7%, p=0.009), flow-limiting dissection (1.4% vs. 6.8%, p=0.03), and provisional stent placement (4.6% vs. 18.3%, p<0.001) were also significantly lower in the IVL group. Secondary outcomes, including rates of MAE and CD-TLR at 30 days, were comparable between groups.
The Disrupt PAD III study provides the largest level I evidence for the treatment of heavily calcified femoropopliteal arteries, a cohort often excluded from endovascular treatment studies. IVL resulted in improved procedural success compared to PTA prior to DCB treatment, demonstrating better lesion dilatation, lower dissections and reduced the need for provisional stent placement.
About VIVA Physicians
VIVA Physicians, a not-for-profit organization dedicated to advancing the field of vascular medicine and intervention through education and research, strives to be the premier educator in the field. Our team of specialists in vascular medicine, interventional cardiology, interventional radiology, and vascular surgery is driven by the passion to advance the field and improve patient outcomes. Educational events presented by VIVA Physicians have a distinct spirit of collegiality attained by synergizing collective talents to promote awareness and innovative therapeutic options for vascular disease worldwide. To learn more about VIVA Physicians, visit www.vivaphysicians.org.
SOURCE VIVA Physicians
For further information: press@vivaphysicians.org
